The Brachytherapy Innovation Team
BC Cancer Agency Southern Interior (CSI) is home to an active Brachytherapy Innovation Team of inspired Medical Physicists, Radiation Oncologists and Radiation Therapists. This team is a proven leader in brachytherapy development and research in Canada and CSI is currently the only center in British Columbia to offer several advanced brachytherapy treatment options for prostate, gynecological and breast cancer.
Brachytherapy, High-Dose Rate (HDR) or Low-Dose Rate (LDR), is a highly specialized type of therapeutic radiation that offers incomparable precision and radio-biological advantages over External-Beam Radiotherapy (EBRT). It is currently used at CSI to treat gynaecological, genito-urinary and breast malignancies.
Other cancers sites potentially suitable for brachytherapy include skin, oesophagus, head and neck, sarcoma and rectum. It is considered part of the standard armamentarium for treatment of several types of cancer and for some is an essential treatment component for cure. Brachytherapy requires a multidisciplinary team in which Medical Physicists play a key role both clinically and in spearheading technical research and development.
Research Focus in Brachytherapy
Brachytherapy research at CSI is focused on the development and implementation of tools and techniques for precision image guided brachytherapy (IGBT) and dose monitoring. IGBT is the future of brachytherapy as it is the only way that brachytherapy can achieve its full potential of being highly localized and conformal. Research is ongoing in the treatment of breast, cervix, vagina and prostate cancers using both low dose-rate (LDR) seed implant brachytherapy (Prostate, Breast) and high dose rate brachytherapy (Breast, Cervix, Vagina, Prostate) techniques. Several areas of interest are outlined here.
Permanent Breast Seed Implant Brachytherapy
Permanent breast seed implants (PBSI) is a novel, highly attractive treatment for women with early stage breast cancer that is completed in a single out-patient session. The technique involves permanently implanting small radioactive sources into the breast in a single out-patient session. However, PBSI is very challenging and relies heavily on expert practitioners. The Brachytherapy Innovation Team is focused on developing a treatment process that improves accuracy, reduces user dependence and can, ultimately, be implemented widely. A significant focus of this work is in the development and utilization of ultrasound tools for precision IGBT in PBSI. Some recent/future projects include:
- Quantification of seed placement accuracy in PBSI
- Use of US in PBSI treatment planning
- Metrics for measurement of skin dose in PBSI
- Deformable image registration for defining the post-operative seroma in PBSI
- Quantification of seed migration in PBSI
- Implementation of 3DUS for implant guidance
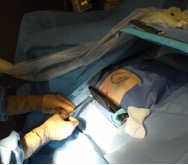
Template and US guided permanent breast seed implant (PBSI) treatment.
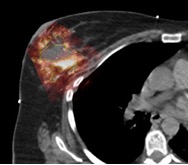
Observed differences in the seroma contoured using CT (yell) and US (green).

Testing a breast ultrasound system for use in permanent seed brachytherapy.
Dose Tracking in Cervical Brachytherapy
The team has recently been investigating tracking the dose delivered to organs at risk over multiple fractions of treatment in cervical brachytherapy. 3D imaging has greatly improved the conformality of HDR brachytherapy. MRI imaging fused to planning CTs allows the actual tumour to be contoured and targeted and 3D CT imaging allows all neighbouring organs at risk (rectum, sigmoid, bladder, small bowel) to be monitored and spared as much as possible. HDR brachytherapy for cervix is delivered in 3-5 fractions and at the moment organ doses are assessed simply by summing the dose each gets each fraction. This assumes that the same portion of each organ is maximally irradiated each fraction. Using deformable images registration tools we can now track where the maximally irradiated portion of each organ actually is from fraction to fraction and determine what the true dose maximum dose to each organ is. This aids in understanding what organ doses are actually delivered and thereby may enhance our understanding of what dose levels correlate with normal tissue complications.
Improved Imaging for Gynaecological Brachytherapy
The brachytherapy team at CSI is committed though research and development to advancement of HDR brachytherapy treatments for gynaecological cancers.
One arena is improving image guidance for interstitial gynaecological brachytherapy. The team at CSI has pioneered an interstitial technique that mimics prostate brachytherapy by mounting an ultrasound probe and template on a prostate stepper and performing trans-vaginal ultrasound (US) imaging during needle implant. This is, however, still limiting due to the 2D nature of the intra-operative imaging, the variable visibility of the target on US, and the fact that we cannot image above the vaginal vault, restricting the number of patients we can treat with this technique. In collaboration with Dr Aaron Fenster of the Imaging Research Labs, Robarts Research Institute, London, Ontario, the team at CSI proposes to develop a system to fuse pre- operative magnetic resonance images (MRI) (where the target is fully visible) to 3D intra-operative US images. This technique will incorporate needle tracking technology allowing better assessment implant quality before imaging for planning. The possibility of combining different US modalities intra- operatively will also be explored; for instance, using both front-firing and side-firing transducers to image above the vault as well as along the length of the vagina. Incorporating Doppler imaging to better identify the target will also be explored.
Another arena for improved imaging in gynaecological brachytherapy is in visualization of the wall of the vagina, an often ignored organ at risk in gynaecological brachytherapy. Vaginal side effects have a large impact on patients’ quality of life following treatment and vaginal stenosis makes follow up exams difficult and painful. This group seeks to investigate a means of identifying the vaginal wall in imaging that can be routinely applied in the clinic. This will facilitate a retrospectively review of the doses delivered to the vaginal wall during treatment for cervix cancer and an investigation of any correlations between dose and complications. Further, we aim to develop a means of routinely prospectively monitoring vaginal wall dose.
Advancing Prostate Brachytherapy
The brachytherapy team at CSI is the only group in BC that offers HDR brachtherapy as a treatment option for prostate cancer. Research is clinically focused on improving HDR prostate treatment strategies and monitoring treatment dosimetry. Recent investigations include integrating a boost dose to the dominant intra-prostatic lesion into the ultrasound based planning and treatment approach used at CSI via “dose painting”.